Introduction:
Teclistamab, a first-in-class B-cell maturation antigen (BCMA) x CD3 bispecific antibody with a personalized, weight-based dosing schedule, gained US regulatory approval in October 2022 for the treatment of triple-class exposed relapsed/refractory multiple myeloma (MM). Teclistamab administration is initiated with a step-up dosing (SUD) period, which includes two step-up doses followed by the first treatment dose. In a prior analysis of 40 patients, we found that early initiators of teclistamab were elderly, diverse, and had significant comorbidities, yet most of the patients completed SUD without delay (Tan SOHO 2023). To continue describing the real-world profile of patients initiating this novel therapy, we updated the prior analysis with a larger sample size and more data. This updated analysis revisited outcomes reported previously, including patient characteristics and SUD process, and evaluated the incidence and management of cytokine release syndrome (CRS) observed in the real-world United States (US) hospital setting.
Methods:
This was a real-world, retrospective, observational study using the Premier Healthcare Database, a hospital chargemaster database covering approximately 20% of US hospitals. We identified hospital encounters with ≥1 teclistamab administration between November 1, 2022 and April 1, 2023, with the earliest encounter as index. To be included, patients were required to have ≥1 diagnosis of MM (International Classification of Diseases, 10 th Revision, Clinical Modification [ICD-10-CM]: C90.0x) on or prior to index, ≥18 years of age on index, and no evidence of clinical trial engagement on or after index. We descriptively analyzed characteristics across all patients in the study, and SUD patterns and CRS in those who completed SUD. CRS was identified in two ways: ICD-10-CM codes and a published algorithm of CRS-related symptom and treatment codes (Keating algorithm).
Results:
A total of 113 patients with ≥1 teclistamab administration were included. Median (interquartile range) age was 65.0 (58-74) years; 21.2% were age ≥75 years; 61.1% had Medicare insurance. Most were male (61.1%), White (65.5%), and non-Hispanic (82.3%), with 21.2% Black. Most patients were treated at urban (97.4%) teaching hospitals (84.1%) with ≥300 beds (89.4%). During hospital encounter for SUD, 62.0% of patients had documented hypertension, 57.5% had anemia, 38.9% had renal impairment/failure, and 36.3% had peripheral neuropathy.
Of 88 patients with available dose strength data, 58 (65.9%) completed SUD by data cut-off, with all SUD doses administered in one inpatient admission. Similar to the prior report, the mean (standard deviation) length of stay was 8.6 (1.7) days after omitting extreme outliers. Most patients had a 3-day (39.7%) or 2-day (20.7%) interval between SUD doses.
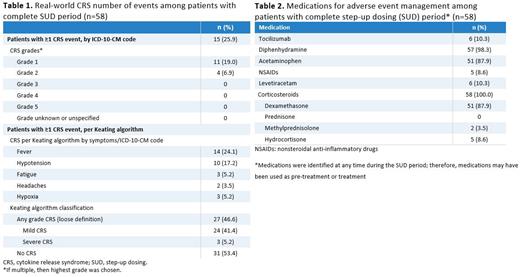
Among the 58 patients who completed SUD, 25.9% of patients had an ICD-10-CM diagnosis code for CRS, with 19.0% with grade 1 and 6.9% with grade 2 as the highest grade. Per the Keating algorithm, 46.6% of patients experienced CRS-related symptoms, and a majority (41.4%) were classified as mild CRS. The most common symptoms indicative of CRS were fever (24.1%) and hypotension (17.2%) (Table 1). At any time during SUD, 10.3% patients received tocilizumab, 100% received corticosteroids, and 87.9% received acetaminophen (Table 2).
Conclusion:
This updated analysis of the first national real-world study of teclistamab confirmed that these initial patients were diverse, elderly, and had significant comorbidities, and most completed SUD without delay. Additionally, fewer than half of patients in this real-world cohort experienced CRS, as identified using ICD-10-CM codes. Limitations of our analysis include the small sample size, reliance on chargemaster data with inherent limitations (e.g., misclassification and coding errors), and the estimation of CRS incidence and management using diagnosis codes. However, this is the largest, real-world hospital-data analysis of patients initiating teclistamab within the first 5 months of market availability. Further updates are needed to augment the data with more patients and longer follow-up time.
Disclosures
Tan:Sanofi: Honoraria; Janssen: Current Employment, Honoraria, Research Funding; Takeda: Research Funding. Kim:Janssen: Current Employment. Chinaeke:Janssen Scientific Affairs, LLC: Current Employment. Hester:Janssen R&D, LLC: Current Employment, Current equity holder in publicly-traded company. Fowler:Janssen: Current Employment. Gifkins:Janssen R&D, LLC: Current Employment, Current equity holder in publicly-traded company. Lin:Janssen Scientific Affairs, LLC.: Current Employment, Current equity holder in publicly-traded company. Walker:Janssen Scientific Affairs, LLC: Consultancy, Current equity holder in publicly-traded company, Ended employment in the past 24 months. Fu:Johnson & Johnson: Current Employment, Current equity holder in publicly-traded company. Wu:Janssen Scientific Affairs, LLC: Current Employment, Current equity holder in publicly-traded company.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal